Nate Weddle has struggled with heroin addiction for years. He first came to Manchester about four years ago to live in a sober house, and did well there. But moving out on his own was harder than he thought. Since then, he’s gone back and forth between relapse and recovery.
“I’m typically proud to be in recovery,” he said. “But unfortunately I’m on the flip side of it now.”
Lately, he’s noticed that some heroin has an unusual effect on him. It’ll knock him out immediately, and he won’t wake up for hours. Weddle, who is 33, has been living on the street, where passing out suddenly can be dangerous. He’s woken up to find his stuff stolen.
Strange skin wounds have also appeared on his hand and arm, in places he wasn’t injecting. The round, scabby sores looked almost like cigarette burns.
“And over time, they actually grew in size and got bigger,” he said.
Health workers are seeing similar symptoms in people across New Hampshire, and they suspect the cause is a substance called xylazine — an animal tranquilizer that's increasingly finding its way into street drugs across the country. Analysts at New Hampshire's state crime lab estimate they’re finding it in about 15% of the fentanyl they test.
Sometimes called “tranq dope,” xylazine-laced fentanyl is creating new hazards for people who use drugs.
It’s the latest turn in a rapidly changing drug supply, in which fentanyl is turning up in everything from cocaine to fake pills, meth use has spiked and any of those substances could be cut with unknown additives. Harm reduction workers in New Hampshire say the state could be doing more to warn people about those kinds of risks.
Ryan Fowler, a harm reduction coordinator with the Lebanon-based HIV/HCV Resource Center, said the unpredictability makes things even riskier for people using already dangerous drugs. Most of the time, they just don’t know what they’re getting.
“It’s kind of Russian Roulette with the drug supply that’s out there,” he said.
Sedation, amputation and other risks

Xylazine has been present in the drug supply in Puerto Rico and Philadelphia for years, but is now increasingly spreading to other parts of the country. Experts say it’s likely being added in to prolong the effects of fentanyl, which has a shorter-lived high than heroin.
Analysts in Massachusetts were finding xylazine in about 30% of heroin and fentanyl samples as of the first half of last year. The tranquilizer was also present in more than a quarter of fatal opioid overdoses in Vermont between January and September.
Health workers on the ground in New Hampshire say they began seeing symptoms they associate with xylazine over the past year or so.
“We started just seeing people that were really, really kind of catatonic, unresponsive. Hearing stories of people who were like, ‘Yeah, I used and then I slept like all day long and I just couldn’t get up,’” said Andrew Warner, who has been doing street outreach in Manchester for several years and now works as the city’s director of overdose prevention. “And that’s not normal.”
Health experts say that kind of prolonged, heavy sedation can cause dangerous circulation problems and make people more vulnerable to crime and harsh weather, especially if they’re unhoused.
Several people in Manchester told NHPR they sometimes fall unconscious suddenly after using drugs.
“I'll wake up on the ground and don't know how I got there, or I'll wake up falling down and hurting myself,” said James, a city resident.
“We’re seeing these horrific wounds across New England right now. And it leads to things like amputation, long-term ICU admissions for IV antibiotics.”Stephen Murray, an overdose researcher at Boston Medical Center
Xylazine can also cause aggressive skin lesions that quickly turn necrotic. Some wounds get so bad they require amputation.
“We’re seeing these horrific wounds across New England right now,” said Stephen Murray, an overdose researcher at Boston Medical Center. “And it leads to things like amputation, long-term ICU admissions for IV antibiotics.”
John Burns, the director of SOS Recovery — which has locations in Rochester, Dover and Hampton — has heard similar stories of people becoming unusually lethargic in his part of the state. He’s also seen severe skin wounds that he thinks could be related to the tranquilizer.
“I’ve seen some wounds that have gone down to the tendon, that you just never see with standard injection drug use of heroin and fentanyl,” he said.
With xylazine and other unknown substances circulating, harm reduction workers are telling people to use smaller amounts, test out new batches with tiny doses and make sure someone else is around when using, so they can administer the overdose-reversal drug naloxone and perform rescue breathing in case of an overdose. It’s also important to get skin wounds treated quickly.
Megan Reed, a professor in the department of emergency medicine at Thomas Jefferson University in Philadelphia, said fentanyl cut with xylazine is changing what overdoses look like.
Naloxone, also known by the brand name Narcan, is still critical to counteract the fentanyl and help restore breathing. But it won’t necessarily wake someone up right away if they’re also under the effects of a tranquilizer — something that’s important for first responders to recognize.
“So the person who overdosed may be breathing [again], but they may still be heavily sedated and not be conscious,” she said. “That person might still be seen to be overdosing and be given a lot more naloxone than they actually need.”
Health workers say New Hampshire lags behind neighboring states in its response

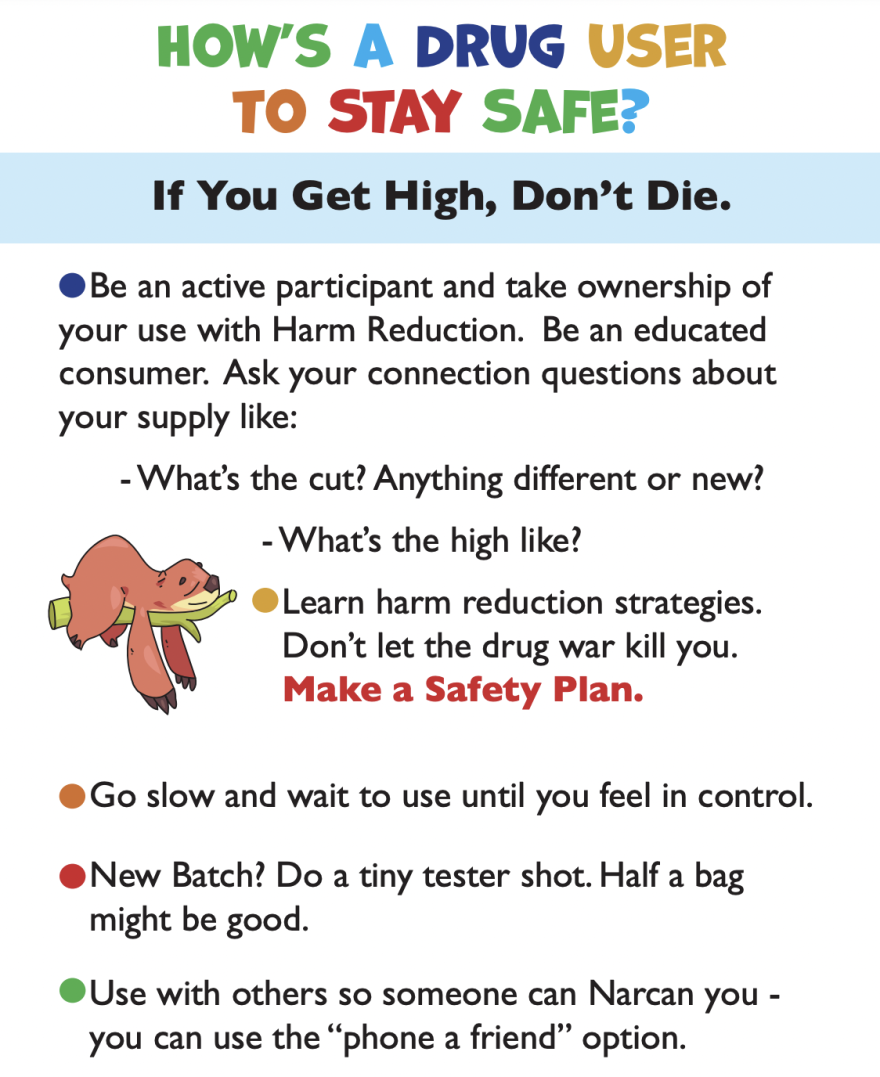
Fowler, the harm reduction coordinator in the Upper Valley, has been trying to warn people about the dangers of xylazine. He’s even created a colorful flier with info about the tranquilizer and safety tips.
He works in both Vermont and New Hampshire, and says the Green Mountain State has been more proactive when it comes to getting the word out. Vermont’s health department issued an alert about xylazine last year and includes data about the drug in its monthly overdose reports.
The New Hampshire Department of Safety sent a warning to the state’s EMS providers about xylazine earlier this month, but there’s been no similar notice to the general public. The Department of Health and Human Services also hasn’t issued any public warnings.
Jake Leon, the health department’s communications director, said the safety department handles alerts about street drugs, but health officials have been communicating with the state’s addiction-treatment hubs and community providers about xylazine.
Still, Fowler says New Hampshire could be doing more to keep people informed about new substances entering the drug supply. One model he and other harm reduction workers point to is Massachusetts, where a network of state-funded drug-checking sites allow people who use drugs to bring them in for testing.
Public health researchers have used that data to issue alerts about the spread of xylazine and track other adulterants like phenacetin, a fever and pain reliever pulled from the market decades ago that has shown up in some cocaine.
Traci Green, a professor at Brandeis University and the drug-checking program’s lead investigator, says that gives people who use drugs a better understanding of the risks they may face. It also helps inform the health workers and first responders on the front lines of the overdose crisis.
“People for their own consumer safety deserve to have access to that information,” she said. “And we as public health and public safety can better respond if we know what we're dealing with.”
New Hampshire, by contrast, puts out little detailed, real-time information about what’s in the drug supply. Harm reduction workers say that leaves them relying on data from other states and their own anecdotal observations as they try to warn people about what’s out there.
“When you tell people about what’s going on and you have real concrete evidence, we’ve seen that people will tend to do things differently,” Warner, the overdose-prevention director in Manchester, said. “But when it’s kind of just this gray area of, ‘You know, I don’t know what’s going on, but something weird is going on,’ it’s much harder to get people to change their behavior.”
While cheap test strips are available to check for the presence of fentanyl, there’s nothing like that for xylazine so far. Burns, of SOS Recovery, said launching a more sophisticated drug-checking program in New Hampshire wouldn’t just require funding — it would also likely require some new legal protections, so workers handling samples are not at risk of arrest. In Massachusetts, he said, many local police departments have agreements with drug-checking sites.
With more accurate information about which substances might be circulating at any given moment, Burns said outreach workers would be more prepared to talk to people about ways to reduce their risk of overdose and protect their health.
Drug checking can be “an awareness and educational tool that helps prevent overdose and helps prevent harms to people who use drugs,” he said. “Because we know that if we don't keep them alive, they're never gonna find their way to recovery.”
Nate Weddle says it would help him and others struggling with addiction to know which batches circulating in Manchester contain unfamiliar substances. That way they could avoid them altogether.
“It’s unfortunate, we’re all kind of identified as hopeless folks that are destined for death on the streets or incarceration for the rest of our lives, just due to the nature of the way that we live,” he said. “But we’re all good people. We’re all normal people.”
He says recovery is still a goal for him — and he’s trying to get back into treatment.





